Abstract
Background:Standard treatment for patients with diffuse large B-cell lymphoma (DLBCL) consists of R-CHOP-21, established when two randomised trials did not find dose-dense administration of R-CHOP to be superior (Cunningham et.al 2013, Delarue et.al 2013). In both these trials, as well as in the majority of other clinical trials that provide the current evidence base for use of R-CHOP-21, 8 cycles of R-CHOP-21 were administered. An exception is the MInT-study, where 6 cycles of R-CHOP-21 was associated with superior outcome to 6 cycles of CHOP-21 for low-risk patients aged <60 (Pfreundschuh et.al 2006). Despite a lack of solid evidence to support the use of 6 instead of 8 cycles of R-CHOP-21 for all patients, administration of 6 cycles is commonly utilised in practice. Also, this strategy is supported by the European Society for Medical Oncology (ESMO) and National Comprehensive Cancer Network (NCCN) guidelines (Tilly et.al 2015, Zelenetz et.al 2016). The NCCN guidelines motivate the use of 6 cycles for all patients partly by the increased toxicity in absence of clinical benefit seen on administration of 8 cycles compared to 6 cycles of dose-dense R-CHOP-14 among patients aged 61-80 in the RICOVER-60 trial (Pfreundschuh et.al 2008).
To our knowledge, no randomised trial has demonstrated superiority of 8 compared to 6 cycles of R-CHOP-21. As part of a current project on utilising real world data from the Danish and Swedish lymphoma registries to predict outcome in DLBCL, we examined whether patients treated with 6 or 8 cycles of R-CHOP-21 had similar survival and could be analysed as a single group.
Methods: The study population was identified through the Swedish and Danish Lymphoma Registries 2007-2015. Patients with leptomeningeal-, eye- or CNS involvement were excluded. Data was conditioned to reach 200 days overall survival to minimise the risk of immortal time bias. Multivariate cox regression analysis included number of chemotherapy cycles administered, age, Ann Arbor stage, performance status, elevated lactate dehydrogenase (LDH), gender and involvement of more than one extranodal site. Sensitivity analyses with patients stratified according to low or high risk, age >/≤70 and excluding patients treated with consolidative radiotherapy were performed.
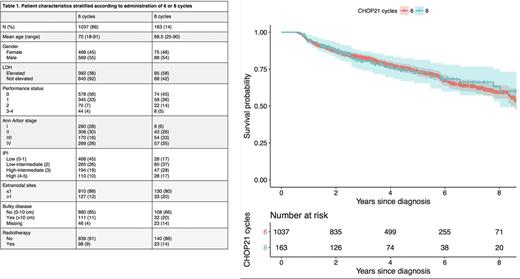
Results:During the time-frame of this study, a total of 1200 adult patients received 6 or 8 cycles of R-CHOP-21 in Sweden and Denmark. Of these, 1037 (86%) were administered 6 cycles, and 163 (14%) received 8 cycles. Mean age was 70 years (range 18-91) in the cohort who received 6 cycles, and 68.5 years (range 25-90) for patients treated with 8 cycles. Radiotherapy was administered to 121 (10%) patients. A larger proportion of patients who received 8 cycles of R-CHOP-21 presented with Ann Arbor stage III-IV, performance status >1, elevated levels of LDH and thus a higher IPI-score (Table 1). Conditional 5-year overall survival rates were 73% in both treatment groups (Figure 1). No difference in outcome was detected for patients administered 6 versus 8 cycles of R-CHOP-21 in a multivariate analysis (hazard ratio: 0.86, 95% confidence interval: 0.62-1.20, p=0.36). Additionally, consistent results of no difference were observed in all patient subgroups stratified according to age (>/≤70), IPI (low/high) or no radiotherapy.
Conclusion: Based on these real world data, we note that the majority of patients with DLBCL treated with R-CHOP-21 during the surveyed time period received 6 cycles, and conclude that the outcomes of patients treated with 6 cycles of R-CHOP-21 were non-inferior to the outcomes of patients treated with 8 cycles of R-CHOP-21.
Figure 1. Overall survival for patients treated with 6 (red line) and 8 (green line) cycles.
Jørgensen: Roche: Research Funding. Smedby: Janssen: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees. El-Galaly: Takeda: Other: Travel funding; Roche: Other: Travel funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal